Ok, so it’s not really ‘alive’ as in the creature from the 80’s movie Aliens starring Sigourney Weaver. But permit a little leeway for hyperbole because I may just change your mind about how you perceive this seemingly inert blob that we call adipose.
I fear that the image in our minds eye of the yellowish-orange blob instructional model shown to us by well-intended teachers or healthcare professionals has helped shape an erroneous perception of this tissue.
These firm but quasi-gelatinous “1 pound of fat” models create the perception that adipose is simply a slumberous, rubbery, and unwanted squatter that seems to have something personal against the waistband of my favorite pair of old jeans (and for some odd reason, every time I see one of these things I get the child-like urge to chuck it like a football).
Having said that, the blob does impart a rather indelible repulsiveness that we would rather forget as we look in the mirror. But therein lies the problem: we think of adipose chiefly in terms of what we see on our exterior.
But would my attitude toward this unwanted house guest change if I were aware of its internal activity, not merely how it looks on the outside? I think the answer is ‘yes’. That’s at least my experience in having the opportunity to work on some of the leading obesity therapeutic drug development programs in the world.
I have become an unwitting expert about, well, that yellowish-orange blob…and let me tell you about its secret: it’s more alive than you can possibly imagine.
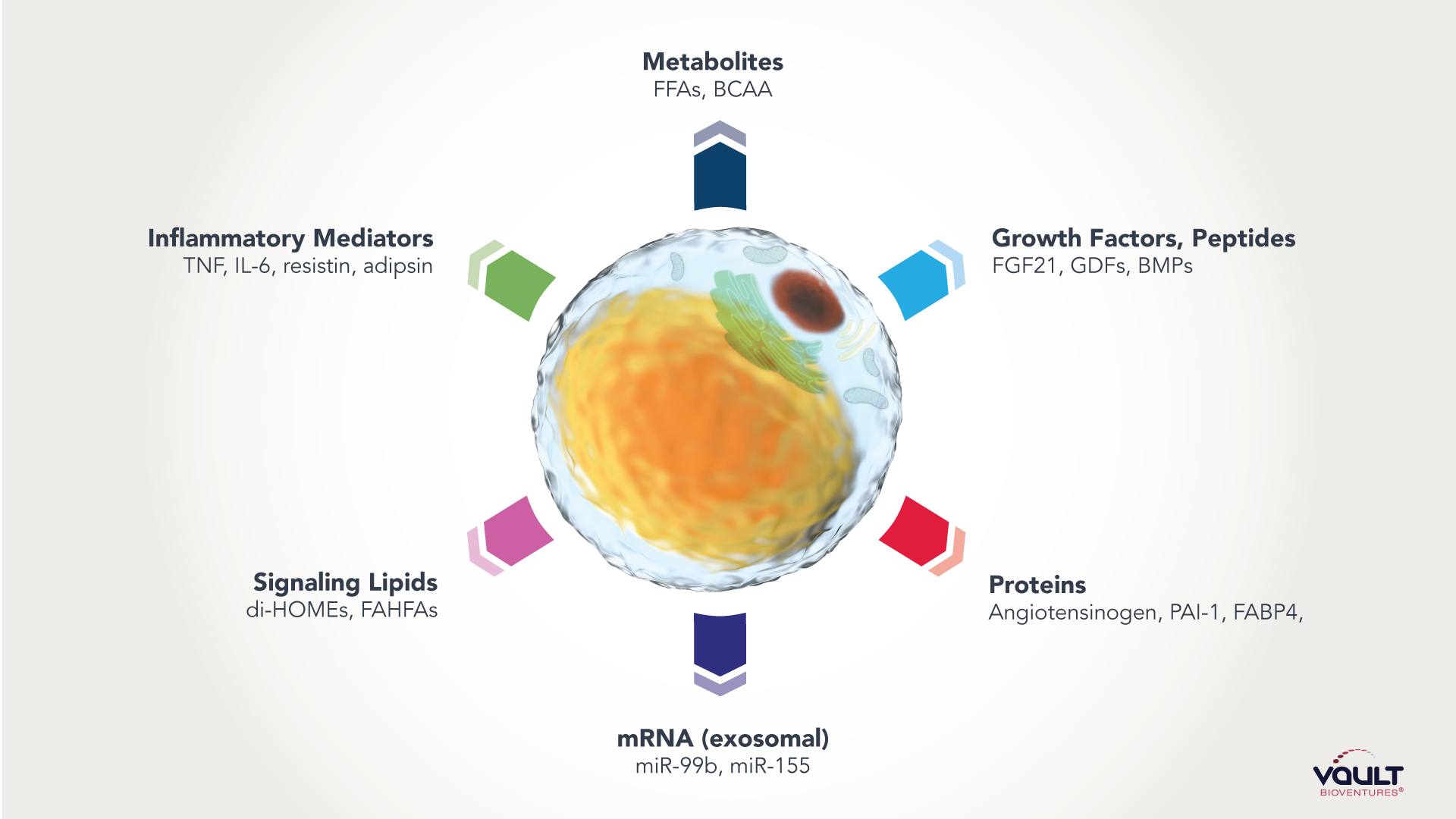
As obesity rates steadily climb across the globe (and especially here in the US), it’s imperative that those of us in the life sciences appreciate the nature of adipose and see it for what it really is – a bustling nest of cells that secrete a mélange of hormonal messengers1 that send signals to targeted organs (have you ever heard of fatty liver disease?2 Fatty pancreas? Fatty kidney?), aiding and abetting metabolic disorder on the inside of your body.
Wait a second, did you say 'secretions that communicate?'
This is where things get interesting.
Adipose also has neural innervation. The prevailing thought was that these nerves were part of the sympathetic nervous system, essentially working only to turn on fat-burning processes when the body needs it. (Recall that the sympathetic nervous system is a system of nerves that is activated in times of stress or danger).
Researchers from Scripps Research Institute (incidentally right around the corner from Vault Bioventures) have now changed the way that we look at this tissue, and their discovery was recently published in the August 31st, 2022 edition of Nature.3 4
Their finding? The presence of a sensory neurons in adipocytes. They tracked neural activity from adipose and found around 50% of the signals did not go through the sympathetic pathway but are instead relayed into the sensory neural pathway (specifically the dorsal root ganglia, for the fellow science geeks out there).5 6 7
'So what,' you say, 'does this geekery have any implications?'
Yes, it certainly does. The sensory nervous system is the surveillance system of body. It processes what we sense – vision, hearing, touch, taste, smell, etc.
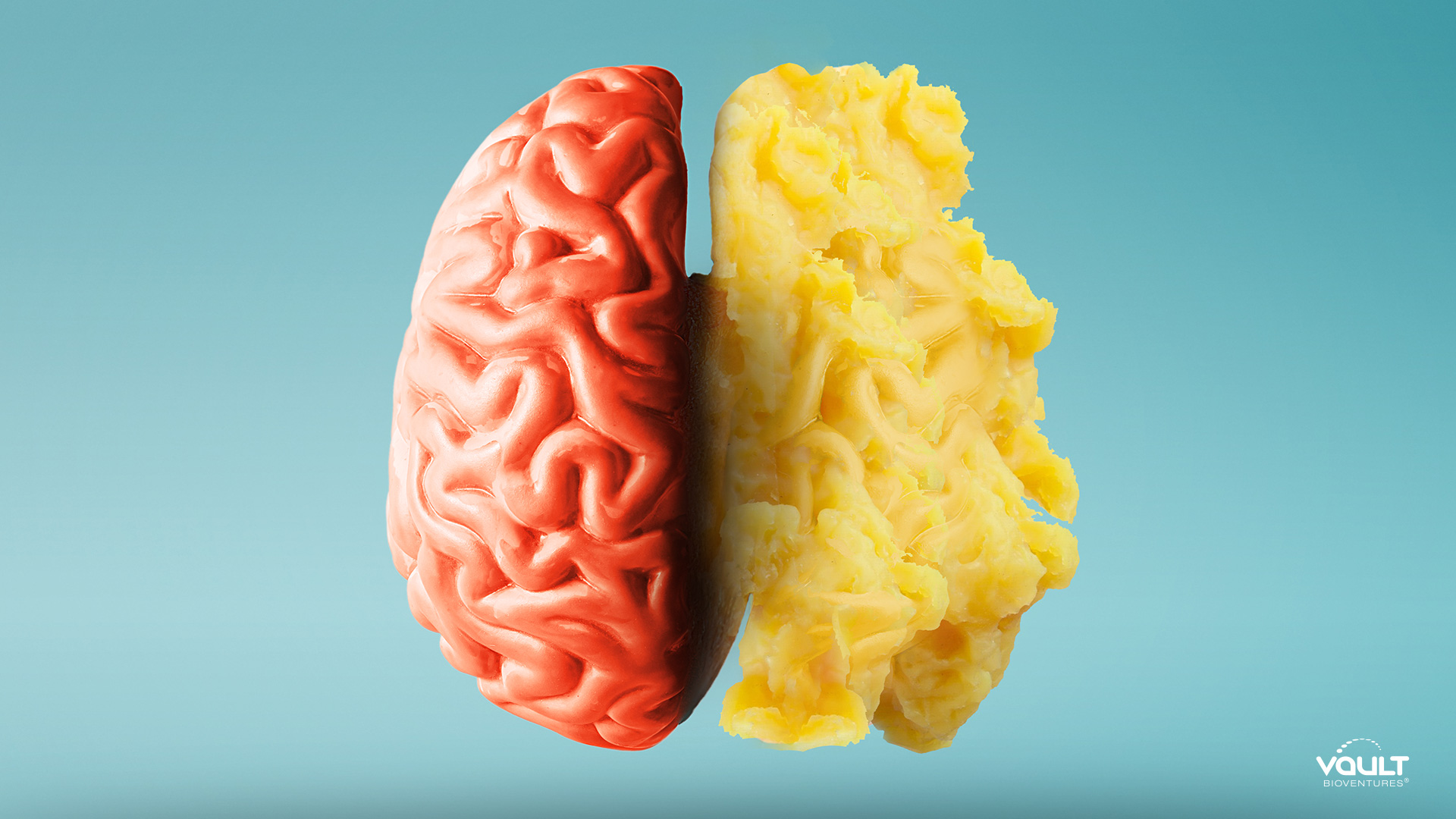
Full stop. Tell me this, could you have conceived that the same neural system that regulates your visual and auditory systems is also ‘listening’, so-to-speak, and responding to your fat???
“The discovery of these neurons suggests for the first time that your brain is actively surveying your fat, rather than just passively receiving messages about it,” explains Li Ye, PhD, one of the study authors in an interview with GEN (Genetic Engineering & Biotechnology News).8
Let that sink in – your brain is actively surveying your fat using the same neural system you are using to read this article.
But Scripps’ findings don’t stop there. They looked at the consequence of disrupting this fat-to-brain sensory pathway and what they found has profound implications: when the sensory nerves were removed in rats, it triggered lipogenesis – the generation of more adipose.
So, whereas the known sympathetic neurons signal lipolysis (fat breakdown) in stress conditions, the sensory nerves seem to serve in an oppositional and homeostatic capacity.
“These two types of neurons are acting like a gas pedal and a brake for burning fat,” explained Ye.9
This discovery will undoubtedly lead Scripps and other scientists in the obesity field closer to lifting the veil on the neural connectivity between tissues, organs, and the brain…and obviously, the implication of pathophysiological changes to these neural systems.
In the meantime, we are left with a multitude of unanswered pragmatic questions:
- As my BMI increases, is there a disruption of the sensory pathway such that lipogenesis is running rampant?
- Are there therapeutic means by which to ‘re-balance’ adipose signaling?
- And why sensory nerves? Why are the same nerves that are used in helping me type this article involved in actually sensing adipose???
We are also left with this: You can erase that image you have of adipose as an inert yellowish-orange blob; the inveterate and dull-witted foe of the waistband.
No, adipose is far more ‘alive’ and active than we had previously imagined. In fact, we are not only looking at it in the mirror – we are also looking at it from the inside.
Perhaps we should consider this when we think that weight loss is simply about ‘will power’ and only a ‘lifestyle’ disease. It appears that people with obesity are facing a far more active internal opponent.
Vault Bioventures, Inc., is a privately held life science consultancy comprised of former pharmaceutical, biotech, medical device and digital therapeutic executives. Metabolics is one of Vault’s core areas of expertise, interest, and research.
For more information on how we can help your organization design and differentiate your products, launch and sustain better brands, or transform and accelerate your business model, email us at: [email protected], or call us at +1 (855) 483-4838.
1Kahn CR, Wang G, Lee KY. Altered adipose tissue and adipocyte function in the pathogenesis of metabolic syndrome. J Clin Invest. 2019 Oct 1;129(10):3990-4000. doi: 10.1172/JCI129187. PMID: 31573548; PMCID: PMC6763230.
2The Cleveland Clinic, Fatty Liver Disease
3Wang, Y., Leung, V.H., Zhang, Y. et al. The role of somatosensory innervation of adipose tissues. Nature (2022).
4Scripps Research press release, Scripps Research scientists eavesdrop on communication between fat and brain, August 21, 2022.
5Wang, Y., Leung, V.H., Zhang, Y. et al. The role of somatosensory innervation of adipose tissues. Nature (2022).
6The Cleveland Clinic, Sympathetic Nervous System
7The Cleveland Clinic, Somatic Nervous System
8Sarkar, Anjali A., PhD. “Fat to Brain Communications Clarified.” GEN – Genetic Engineering & Biotechnology News, published online, September 1, 2022.
9Sarkar, Anjali A., PhD. “Fat to Brain Communications Clarified.” GEN – Genetic Engineering & Biotechnology News, published online, September 1, 2022.
